What is Ulcerative colitis? Symptoms, Causes and Treatment
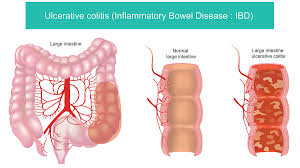
What Is Ulcerative Colitis? Ulcerative colitis is a chronic condition in which the inner lining of your large intestine (colon) and rectum becomes inflamed and develops ulcers. These ulcers can bleed and produce pus. The condition leads to symptoms such as frequent diarrhea, abdominal pain, and urgency. Over time, if untreated, ulcerative colitis can affect your overall health. What Are the Symptoms of Ulcerative Colitis? Common symptoms of ulcerative colitis include: Persistent diarrhea, often with blood or mucus Abdominal cramps, especially in the lower left side A strong, urgent need to pass stool Fatigue, weight loss, and sometimes fever during flare-ups During remission, symptoms may fade but the risk of flare remains If you experience new bleeding, high fever, or severe pain, seek medical care promptly. What Causes Ulcerative Colitis? The precise cause of ulcerative colitis remains unknown, but doctors believe it involves a combination of factors: Genetics: a family history of ulcerative colitis increases your risk. Immune system problems: the immune system may react wrongly and keep the colon lining inflamed. Environmental triggers: infections, diet, stress, and gut microbiome changes may all play a role. Gut bacteria: an imbalance may prompt the immune reaction that drives ulcerative colitis. Is Ulcerative Colitis an Autoimmune Disease? Yes—and sort of. Ulcerative colitis is widely considered an immune-mediated inflammatory disease, which means your immune system plays a major role in causing the inflammation.However, whether it meets the strict definition of “autoimmune disease” (where the body produces autoantibodies that attack its own tissues) is debated. Many doctors classify ulcerative colitis as immune-driven rather than classic autoimmunity. WebMDIn short: if you ask “Is ulcerative colitis an autoimmune disease?” the answer is yes in practical terms, but with some nuance. How Is Ulcerative Colitis Diagnosed? Diagnosis of ulcerative colitis typically involves: Medical history and symptom review (diarrhea, blood in stool, pain) Physical examination Laboratory tests: blood work, stool tests to exclude infection Colonoscopy with biopsy: to see inflammation and ulcers in the colon lining Imaging: sometimes CT/MRI if complications are suspected Early diagnosis helps manage the disease and reduce complications. What Are the Treatments for Ulcerative Colitis? Treatment of ulcerative colitis aims to induce remission, maintain remission, and improve quality of life. Treatments include: Medication: anti-inflammatory drugs (like aminosalicylates), corticosteroids for flares, immune-modulators, biologic therapies targeting specific immune pathways. Lifestyle and diet: changes to avoid triggers, eat well during remission, and manage stress. Surgery: if medications fail or complications occur, removal of the colon may be required; this can lead to a cure of colitis symptoms (since the colon is removed). Regular follow-up: monitoring for colon cancer risk, bone health, nutrient deficiencies. What Are the Worst Foods for Ulcerative Colitis? When you have ulcerative colitis—especially during a flare—certain foods are more likely to worsen symptoms. Here’s a detailed list of worst foods to avoid or limit, with reasons. High-Risk Food Groups Fried, fatty, and processed foodsThese foods are hard to digest and may increase inflammation in the gut lining. Spicy foods and strong seasoningsCapsaicin and strong spices irritate the inflamed colon lining and increase cramping and urgency. High-fiber foods during flaresRaw vegetables, whole grains, nuts/seeds may bulk up stool, cause bloating, and stress the gut when inflamed. Nuts, seeds, popcorn, legumesThese have tough textures or indigestible sugars and are common triggers for flare-ups. Dairy (if lactose intolerance is present)Many with ulcerative colitis also have secondary lactose intolerance when the gut lining is damaged. Sugar alcohols, carbonated drinks, sugary foodsSugar alcohols like sorbitol, xylitol and fizzy/sweet drinks may cause gas, bloating, diarrhea. Red meat and processed meatsHigh fat and tough protein make them harder to digest and may worsen inflammation. Practical Avoidance Tips During a flare: choose low-residue meals (white rice, peeled cooked veggies, lean cooked poultry/fish). Keep a food diary: note what you eat, how you feel afterwards, to detect your own triggers. When in remission: gradually reintroduce foods one at a time and see how your body reacts. Consider speaking with a dietitian experienced in IBD for personalised guidance. What Are the Best Foods and Diet Tips for Ulcerative Colitis? While many foods may trigger symptoms, you can focus on softer, easily digestible, nutrient-rich foods, especially during flares. Some helpful tips: Eat smaller meals 4-6 times per day rather than large meals. Mayo Clinic Choose cooked, peeled, skinless vegetables (carrots, zucchini), white rice or low-fiber grains. Lean proteins: skinless poultry, fish, eggs (if tolerated). Hydrate well: diarrhea can lead to dehydration and electrolyte imbalance. When in remission: include whole fruits/vegetables gradually, healthy fats (olive oil, fish), and fibre slowly — monitor your response. Avoid eating right before bed, reduce stress, get good sleep — all of which help gut health indirectly. What Are Complications and When to Seek Help in Ulcerative Colitis? If you have ulcerative colitis, you should watch for and discuss with your doctor: Severe bleeding, persistent high fever, dehydration, or symptoms of toxic megacolon (a life-threatening dilation of the colon). Increased risk of colorectal cancer — long-standing ulcerative colitis raises this risk, so regular colonoscopy surveillance is important. Malnutrition, nutrient deficiencies (iron, vitamin D, B12) due to chronic inflammation or frequent diarrhea. Extra-intestinal complications: joint, skin, eye, liver issues connected with ulcerative colitis. Impact on quality of life: fatigue, emotional burden, and the need for mental-health support. Frequently Asked Questions about Ulcerative Colitis Q: Can ulcerative colitis be cured?A: Not by standard medication alone, but if the colon is removed surgically, the disease in the colon is effectively eliminated. Most treatment plans aim for remission not “cure.” Q: Is ulcerative colitis the same as Crohn’s disease?A: No; both are inflammatory bowel diseases, but ulcerative colitis affects only the colon/rectum lining, while Crohn’s Disease can affect any part of the gut and deeper layers. Q: Do I have to avoid all fiber forever with ulcerative colitis?A: No. During flares it’s wise to avoid high-fibre/insoluble foods. But during remission, gradual reintroduction of fibre is possible—many professionals recommend doing so with caution and watching symptoms. Q: Does diet alone treat ulcerative colitis?A: No. Diet
What is Ulcerative colitis? Symptoms, Causes and Treatment Read More »